
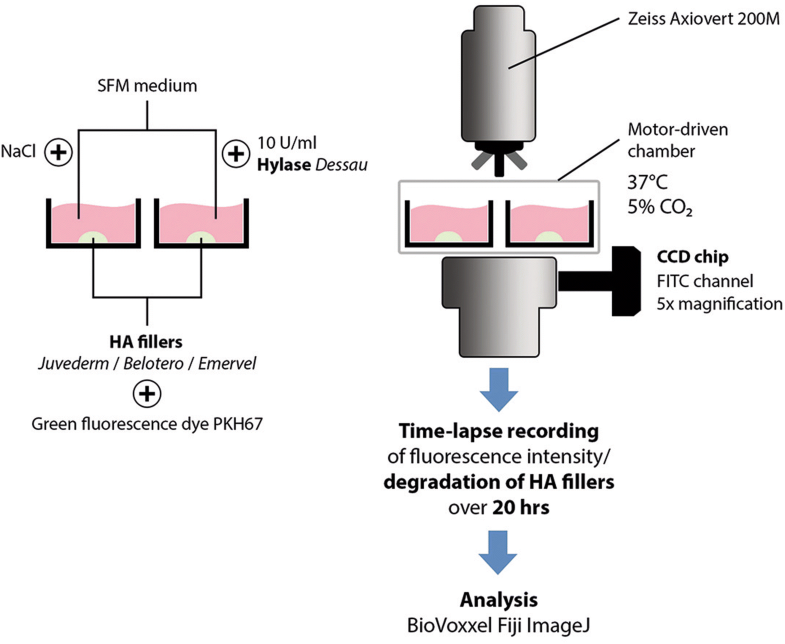
5 Most surgeons are familiar with its use as a local anesthetic additive that facilitates cutaneous dissection via its enzymatic action on native hyaluronic acid found in the extracellular connective tissue matrix. It also breaks down other acid mucopolysaccharides found in connective tissue. Hyaluronidase is an enzyme that depolymerizes hyaluronic acid by cleavage of glycosidic bonds. The key ingredient responsible for cutaneous augmentation with NASHA gel is hyaluronic acid, a natural, high-viscosity hydrophilic mucopolysaccharide with an ability to hold water. Given the long-lasting effects of NASHA gel injection, the resultant iatrogenic deformities could create persistent dissatisfaction in many patients.

1-4Īs with any dermal filler, however, unintended dermal augmentation can occur with NASHA gel owing to overcorrection attempts or injection error. When compared with bovine collagen, NASHA gel has demonstrated longer-lasting dermal augmentation results with significantly lower rates of hypersensitivity reactions. Restylane is a hyaluronic acid–containing gel produced by bacterial fermentation, stabilized by chemical cross-linking, and suspended in a physiologic buffer at a concentration of 20 mg/mL. A 10-year experience with 150 cases.Restylane (Q-Med AB, Uppsala, Sweden), or nonanimal stabilized hyaluronic acid (NASHA) gel is approved by the United States Food and Drug Administration (FDA) for the filling of moderate to severe wrinkles around the nose and mouth, such as nasolabial folds.
#Hyaluronidase vs vtrace trial
INTERPRETATION & CONCLUSION: Treatment regimen of group B was more convenient to the patients because less number of visits required and cheap. RESULTS: No statistically significant difference in symptom score, sign score and histopathological improvement was seen between the two groups. Student's 't' test was applied for comparing the results. Treatment outcome was evaluated on the basis of improvement in symptom score, sign score and histopathological improvement. Group B patients received combination of triamcinolone acetonide (10 mg/ml)/ hyaluronidase (1500 IU) at 15 days interval for 22 wk. Group A patients received combination of hydrocortisone acetate (1.5 ml)/hyaluronidase (1500 IU) at weekly interval submucosally in pterygomandibular raphe, half dose on each side for 22 wk. METHODS: Patients of OSMF (100) were randomly divided into two groups A and B. In this study we compared the efficacy of hydrocortisone acetate and hyaluronidase at weekly interval versus triamcinolone acetonide and hyaluronidase at 15 days interval. The problem with the prevailing treatment was injections at weekly interval. Its medical treatment is not yet fully standardized, although the optimal doses of its medical treatment is in the form of hydrocortisone acetate combined with hyaluronidase. N2 - BACKGROUND & OBJECTIVES: Oral submucous fibrosis is a common premalignant condition caused by chewing arecanut and other irritants in various forms. JF - The Indian journal of medical research T1 - Efficacy of hydrocortisone acetate/hyaluronidase vs triamcinolone acetonide/hyaluronidase in the treatment of oral submucous fibrosis.


 0 kommentar(er)
0 kommentar(er)
